February 21, 2024
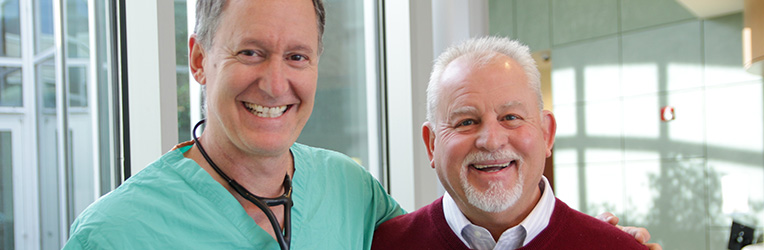
From Crisis to Recovery: A Patient's Story
Gary Morgan suffered a saddle pulmonary embolism, which nearly resulted in his death. But with the help of his surgeon and care team, Mr. Morgan has gone from medical crisis to feeling better than ever before. Read his story.
Recent News
Press Inquiries
CaroMont Health’s Public Affairs Department is available to assist the media in coverage of local, state and national healthcare issues.